My most recent column in the San Francisco Chronicle appeared later than usual (March 14) so I forgot to post it when it came out. It deals with Listeria in pregnancy:
A guide to avoiding Listeria
Nutrition and public policy expert Marion Nestle answers readers’ questions in this monthly column written exclusively for The Chronicle. E-mail your questions to food@sfchronicle.com, with “Marion Nestle” in the subject line.
Q: I miscarried at 19 weeks of pregnancy. My doctor said my placenta was infected with Listeria, only her second case in 20 years of practice. I am your typical Bay Area food lover. I thought if I knew the sources of most of my food, I’d be safe. What is safe for pregnant women to eat in the post-Michael Pollan era?
A: Thanks for allowing your personal tragedy to alert others to this hazard. Losing a wanted pregnancy is a heartbreak. Losing one to a food-borne illness is especially tragic. Such illnesses should be preventable.
Food should be safe before it gets to you. That it sometimes is not is a consequence of our inadequate food safety system, which does not require food producers to test for harmful bacteria. The House of Representatives passed legislation that does so last summer, but the Senate is sitting on it. As an individual, you cannot easily protect yourself against invisible hazards in food. Congress must pass that legislation.
Without federal requirements, you are on your own to keep yourself and your unborn infant safe from food pathogens, especially Listeria. Much as I hate to add to what the French sociologist Claude Fischler calls “Listeria bacteria hysteria,” I must. Listeria preferentially affects pregnant women. If you are pregnant and want to stay pregnant, you must avoid Listeria.
This will not be easy. Listeria is widely dispersed in foods. Infections from it may be rare, but they are deadly. Listeria kills a shocking 25 percent of those it infects and is particularly lethal to fetuses.
Most people, including pregnant women, are immune to Listeria and do not feel ill when infected. But unlike most bacteria, Listeria penetrates the placenta, and fetuses have no immunity. The first sign of an infection can be a miscarriage or stillborn infant – too late for antibiotics.
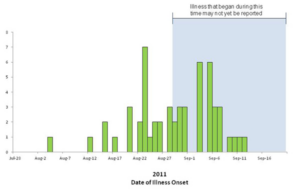
How worried should pregnant women be about Listeria? Given our ineffective food safety system, I’d advise caution. The Centers for Disease Control and Prevention report 2,500 cases a year and 500 deaths. These numbers are minuscule – unless your pregnancy is affected.
Cases occur mainly among the young, the old and others with poor immunity. But the cause of miscarriages is not typically investigated, and I’m guessing that fetal deaths from Listeria are badly underreported.
Animals and people often excrete Listeria from their digestive tracts, even when they show no signs of illness. The bacteria get into food from infected animal waste and unwashed hands.
As a result, unpasteurized milk products and contaminated raw vegetables are frequent food sources. Other sources depend on yet another of Listeria’s nasty features – Listeria grows, reproduces and flourishes at refrigerator temperatures that stop other bacteria cold.
This explains why the CDC strongly advises pregnant women not to eat potentially undercooked foods stored in refrigerators: hot dogs, lunch meats, deli meats, patés, meat spreads and smoked seafood (salmon, trout, lox, jerky); soft cheeses such as feta, Brie, Camembert, those with blue veins, and especially Mexican “queso blanco fresco”; and raw milk or foods containing unpasteurized milk.
Even though some of these foods were cooked or pasteurized to begin with – blue cheese, for example – they can become contaminated after processing. Days or weeks of refrigeration give Listeria ample time to reproduce. Just about any food sitting around in a refrigerated package can be a source, with meat, fish and dairy foods especially suspect.
The CDC advises following safe food handling procedures to the letter at home. Avoid cross-contaminating raw and cooked foods, and use refrigerated perishables right away.
Listeria infections were virtually unknown 25 years ago, so view this hazard as collateral damage from the consolidation and centralization of our industrialized food supply.
Do not despair. There is some good news. Cooking kills Listeria. Pregnant women still have plenty of options for good things to eat that are safe.
Anything cooked hot is safe. So are hard cheeses, semisoft cheeses like mozzarella, pasteurized processed cheeses, and cream and cottage cheeses. These were cooked or are now too dry and salty for bacterial growth. Anything canned – patés, meat spreads, smoked fish, other fish – also is safe.
When it comes to food hazards during pregnancy, Listeria is unique. A sip of wine every now and then is not going to induce fetal alcohol syndrome, nor will your baby get mercury-induced brain damage from an occasional tuna sandwich. The risks from such hazards accumulate with amounts consumed over time.
But the risk from Listeria is acute. With so much at stake, and so many other food choices available, why take chances?
Just last month, the Food and Drug Administration reported recalls of queso fresco, blue cheese and bean sprouts because of possible Listeria risk. The FDA is doing its best, short of legislation. To keep Listeria out of the food supply, Congress needs to act. Write your representatives now.
Marion Nestle is the author of “Food Politics, “Safe Food” and “What to Eat,” and is a professor in the nutrition, food studies and public health department at New York University. E-mail her at food@sfchronicle.com and read her previous columns at sfgate.com/food.