Interview with Scientific American on the complexities of salt science
I complained to Scientific American about one of its blog posts about salt, which I viewed as rather one-sided. The result was a conversation with Michael Moyer that ended up in the form of a Q and A. I did not have a chance to review it before it was posted, so please see addendum at the end).
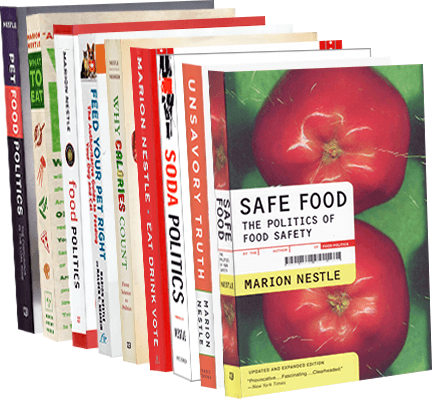
The Salt Wars Rage On: A Chat with Nutrition Professor Marion Nestle
A researcher explains why there may never be a good study on whether excess dietary salt causes hypertension and heart disease
By Michael Moyer | Thursday, July 14, 2011
Is salt bad for us? In just the past few months researchers have published seemingly contradictory studies showing that excess sodium in the diet leads to heart disease, reduces your blood pressure, or has no effect at all. We called Scientific American advisory board member Marion Nestle, a professor of Nutrition, Food Studies, and Public Health at New York University and the author of Food Politics, to help parse the latest thinking regarding salt and heart health.leads to heart disease, reduces your blood pressure, or has no effect at all. We called Scientific American advisory board member Marion Nestle, a professor of Nutrition, Food Studies, and Public Health at New York University and the author of Food Politics, to help parse the latest thinking regarding salt and heart health.
[An edited transcript of the interview follows.]
I understand this area is controversial.
Hugely.
Could you take us through some of the controversy?
If you talk to any kidney specialist or anybody working on hypertension they will tell you that the first thing they do is try to lower the amount of salt their patients are eating because it helps with blood pressure control. But if you do a clinical trial where you try to put large amounts of people on a low-salt diet, you just don’t see much difference between the people who say they eat a lot of salt and the people who say they don’t eat a lot of salt. In clinical trials the relationship doesn’t show up.
Why not?
Two reasons: One that it’s impossible to put a population of people on a low-salt diet. Roughly 80 percent of the salt in the American food supply is in foods before people eat them—either in processed food or in restaurant food. Because so much salt is added to the food supply and because so many people eat out, it’s impossible to find a population of people who are eating a low-salt diet. They basically don’t exist.
In the one comparative epidemiological study they did some years ago—the Intersalt study—they managed to find two populations of people in remote areas of the jungle someplace who weren’t eating a lot of processed foods and who weren’t eating in restaurants. They were on a low-salt diet, and they never developed hypertension.
So in that trial did they put one group on a high-salt diet and put one on a low-salt diet?
No, no, no. It wasn’t a comparative trial. They just looked at the amount of salt that populations were eating and the amount of hypertension that they had. Only in these two populations were there very low rates of hypertension. With everybody else the salt intake was so high that they couldn’t see any difference between high and higher.
So except for people living in the jungle somewhere, there aren’t any populations on Earth that are eating a low amount of salt?
Not anymore. Maybe we used to be, but not anymore. We have a global food supply, so it’s impossible to do a really careful study.
What’s the other issue?
Not everybody responds to a low-salt diet. There’s a proportion of people in the population who are sensitive to salt—if you lower their intake of salt, then their blood pressure goes down. There’s another (probably larger) percentage of the population who doesn’t respond. They are people who can eat as much salt as they want and still their blood pressure is low.
So you have this curious anomaly where whenever you do a clinical trial you get these complicated, difficult-to-interpret results that don’t show much of an effect. But everybody who works with patients who have hypertension think they do better [on a low-salt diet]. And every committee, body, and group that has ever in my lifetime considered whether salt has anything to do with hypertension says, “yes,” and has recommended salt reduction as a public health measure. That’s the curious situation that we are in.
There’s one other wrinkle and has to do with people’s taste for salt. Campbell’s soup, for example, just announced yesterday that can’t sell low-sodium soups and so they’re adding salt back. And part of the reason they can’t sell it is that if you’re on a high-salt diet, food that isn’t salty tastes terrible to you. And if you’re on a low-salt diet it takes three to six weeks to get accustomed to being on a low-salt diet and then everything you eat tastes salty. And so the more salt in the food supply the more salt people need to bring the flavor you associate with salt. That complicates things, too.
So from a public health standpoint, if you want to deal with the percentage of the population that seems to be extremely responsive to a low-salt diet what you want to do is get the sodium level in the food supply as low as you can. And that makes the people who sell salty food go nuts. And it makes the people who like salty foods go nuts. They think the food tastes bland. And so there are different stakeholders in this system who have very different views and that accounts for the level of passion, I think, in a situation where the science is murky.
Couldn’t you just make the case that people should eat fewer processed foods?
Well what about restaurants? I’m a food professional. I eat out professionally.
Well chefs need to make their food taste good—otherwise people won’t go to their restaurant.
No, they need to make the food taste good by their standard. And chefs, because they’re dealing with a great deal of salt in their food, tend to raise the sodium level. It just goes up and up and up and up. As they get more used to a certain level of salt taste it no longer tastes salty to them and they have to raise it. So the pressure is to raise the salt in the food supply. And reducing it is very difficult.
So you advocate regulation to limit the amount of salt in restaurants?
Yeah, I do. Certainly for processed food. I think everybody would be healthier if they ate less salt. You can always add salt if you don’t think it’s salty enough, whereas I can’t take it away if it’s presented to me. And that’s the dilemma. And the ferocity of the arguments gets into the whole question of personal responsibility and “nanny state” and all of these other enormous debates that really don’t get at the public health question. And the public health question is hard to resolve because the science is really difficult to do.
Couldn’t you imagine a study where you look at sodium levels in urine, which is a direct measure of salt intake, and correlate that with hypertension?
Yeah they’ve done that, and they don’t see any difference in hypertension rates. The reason is that the baseline [level of salt intake] is so high that it doesn’t make any difference. To suggest that people get down to 1,500 mg a day—the recommended level—would be really really hard, and that level may be too high. And it’s unclear that that’s the right level because you can’t do a really decent dose response, and because people vary so much.
Will there ever be a good study?
I don’t know!
Is it possible that this represents the limits of science? It’s black hole event horizons and salt intake?
It may be. It very well may be. Or the science that we have is completely adequate and we already have the answer. I was once at a sodium meeting at which there were a bunch of statisticians. And I left with the statisticians and they said that “anyone who thinks that salt has anything to do with hypertension is delusional.” And that was on the basis on the clinical trials that show so little. And yet every single committee that has dealt with this question says, “We really need to lower the sodium in the food supply.” Now either every single committee that has ever dealt with this issue is delusional, which I find hard to believe—I mean they can’t all be making this up—there must be a clinical or rational basis for the unanimity of these decisions.
But that’s the thing—these committees should be able to point to the evidence that supports their recommendations. But they seem to rely so much on anecdote and individual experience.
Or on some clinical trials that everybody argues about. Everybody argues about every clinical trial no matter what the conclusion. So I find the whole thing completely fascinating. I don’t think anybody can underestimate the difficulty of doing nutritional research. Because people aren’t eating just sodium. They’re eating sodium in food. And it may be that high-sodium diets are a marker for some other things in the food supply or it may be that the physiological differences are so profound that you just don’t get clean results. That human variation is so great. I don’t know the answer to that. I just know it works for me. That’s anecdotal. With an “n” of one.
Addendum
If I had been given the opportunity to review this before it was posted, I would have edited it carefully. Yes, this is the way I talk but I don’t think what I said reads clearly in print. In reading over this piece, I think it may give the wrong impression of my views on how expert committees decide on salt recommendations. The piece may give the impression that committees make dietary recommendations basied on anecdotal evidence, not science. That’s not true. They base their recommendations on their interpretation of the experimental and clinical evidence, including that from clinical trials.
For example, the Advisory Committee for the 2010 Dietary Guidelines concluded that “a strong body of evidence has documented that in adults, as sodium intake decreases, so does blood pressure.” Was this committee delusional in viewing the evidence as strong? I don’t think so.