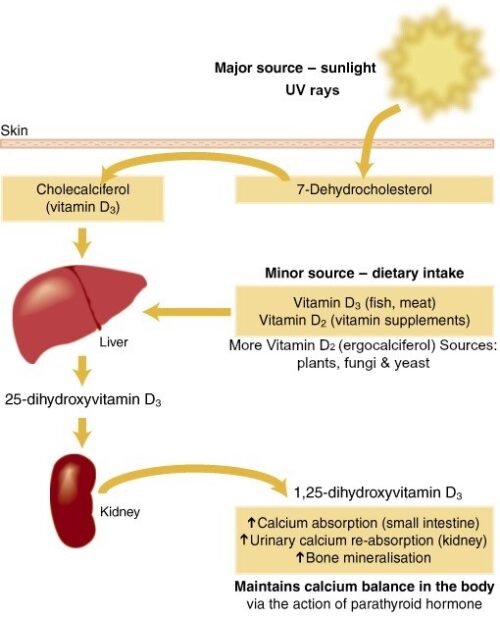
Industry-funded research: Vitamin D and Covid-19
I was interested to come across this paper: Conflict of Interests in the Scientific Production on Vitamin D and COVID-19: A Scoping Review. Front Public Health. 2022 Jul 11;10:821740. doi: 10.3389/fpubh.2022.821740. eCollection 2022.
Results and conclusions:
- Studies were funded by companies in the diagnostics, pharmaceutical and food sectors.
- Conclusions favorable to vitamin D supplementation were more prevalent in papers where COI was identified (9/13, 69.2%) than among papers where COI was not found (4/16, 25.0%).
- Omissions of disclosure of COI, funding source, and sponsor functions were observed.
- The identification of possible corporate political activities in scientific papers about vitamin D published during the COVID-19 pandemic signals a need for greater transparency and guideline development on the prevention of COI in scientific production.
Comment: Not many studies look at disclosure issues this closely. This is a welcome addition to the genre. It reminds me of this especially entertaining report: “COVID-19 and misinformation: how an infodemic fuelled the prominence of vitamin D.” Papers on vitamin D and COVID-19, it seems, are not only influenced by corporate interests; they are also occasionally fraudulent, if viral.
********
For 30% off, go to www.ucpress.edu/9780520384156. Use code 21W2240 at checkout.