I haven’t said anything about the E. coli 0104 crisis in Germany up to now because I’ve been waiting for the evidence. Without evidence, the source of the outbreak remains uncertain.
Yesterday, the German minister of agriculture announced that sprouts are the cause. But are they?
What is known without question is that the outbreak is deadly serious. Bill Marler reports these shocking numbers as of June 5:
Deaths = 22 (21 in Germany, 1 in Sweden)
Illnesses = 2,243 (2,153 in Germany, and 90 more in 10 other European nations and the U.S.)
Cases of Hemolytic Uremia Syndrome (HUS) = 627
Why shocking? This is a devastating disease, excruciatingly painful, with a high probability of causing lifelong complications. And the disease is almost entirely preventable by following standard food safety procedures.
The idea that the cause is sprouts, and German sprouts at that, comes as a surprise. Why? First, sprouts are a frequent cause of foodborne illness and should have been high on the list of suspected foods. Second, sprouts did not turn up in the case-control studies.
Instead, investigators examined cucumbers, lettuce, and tomatoes (and, in the process, put Spanish cucumber producers out of business). As Marler explains, the German authorities didn’t want to take a chance, given the results of their investigation.
The case-control investigation was conducted by the Robert Koch Institute, the German equivalent of our CDC.
- The cases: From May 29 to June 2, investigators interviewed 46 affected patients from Bremen, Hamburg and Lübeck about the foods they had eaten.
- The controls: They interviewed 2,100 people who were not sick but were of similar age group, sex and region of residence.
- The results:
Food Reported Eaten % By Cases % By Controls
Lettuce 84 47
Cucumbers 75 50
Tomatoes 80 63
95% of the Cases had eaten at least one of the three vegetables.
This evidence strongly implicates these vegetables. But did they not look for sprouts?
In another related study of people from a Frankfurt business company who had become ill, those who had eaten from the salad bar in the company cafeteria had a 7-fold increased risk of developing bloody diarrhea than those who had not. No such association was seen for other foods investigated, such as dessert, fruit and asparagus. Sprouts are not mentioned. How come?
In trying to figure out what’s going on here, a BBC World News report raises even more questions (my emphasis):
The agriculture minister for Lower Saxony, Gert Lindemann, said there was a clear trail of evidence pointing to a plant nursery south of Hamburg [as the source of the contaminated sprouts].
The nursery has been closed, though officials say the outbreak’s source cannot yet be definitively confirmed.
…Mr Lindemann said epidemiological studies all seemed to point to the plant nursery in Uelzen in the state of Lower Saxony, about 100km (62m) south of Hamburg – though official tests had not yet shown the presence of the bacteria there.
“Further evidence has emerged which points to a plant nursery in Uelzen as the source of the EHEC cases, or at least one of the sources,” he said. [What evidence?]
…Gert Hahne, a spokesman for the Lower Saxony agriculture ministry, earlier told the Associated Press news agency that many restaurants in which people ate before becoming ill had recently taken delivery of the sprouts. [Guilt by association]
He said authorities would still maintain a warning against eating tomatoes, cucumbers or lettuce.
The health ministry in Berlin said it was still waiting for results from tests on the beansprouts, Germany’s DPA news agency reported.
And the head of the Robert Koch Institute (RKI), Germany’s national disease centre, was also reported as saying that the cause of the outbreak could not yet be confirmed.
So: are sprouts the cause?
By this time, the outbreak is slowing down as the contaminated foods make their way through the food supply.
Could this happen here? You bet.
If ever there was a time to give the FDA more resources, now is it. The FDA now has the authority to impose standard food safety procedures on food producers and to require safety measures for the foods we import. But Congress wants to cut the agency’s budget, and badly.
Now would be a good time to let congressional representatives know that we need a stronger FDA. And while you are at it, let the USDA know that you think it would be a good idea to regulate other forms of toxic E. coli as adulterants in the same way they regulate E. coli 0157:H7. There is plenty government could do right now to protect us from outbreaks like this one.
A word about sprouts:
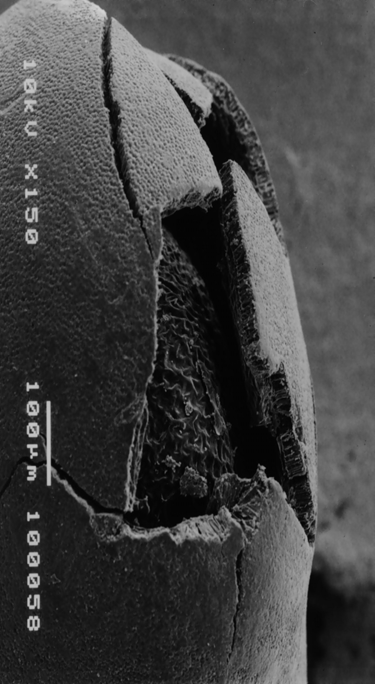
How come sprouts are such frequent sources of food safety problems?
Sprouts are grown from tiny seeds that are impossible to wash thoroughly enough to ensure that they are free of harmful bacteria. The seeds are sprouted in water that must be changed several times a day. This water is an excellent growth medium for bacteria. That is why FDA guidance says sprout producers ought to test the wash water for harmful bacteria.
Under the new legislation, the FDA has the authority to enforce this guidance. But does it have adequate personnel? Unlikely, given the current stance in Congress.
This just in: No, it’s not sprouts, according to this bulletin from Food Chemical News:
The latest news, reported this morning by both the Associated Press and BBC, is that 23 of 40 samples of organic sprouts taken from the Gaetnerhof farm in the Lower Saxony region of Germany have tested negative for the bacteria. Tests on the other samples have yet to be returned.