Thoughts about nutrition II. The need for leadership
II. The need for nutrition science leadership in promoting policies to prevent and treat disease
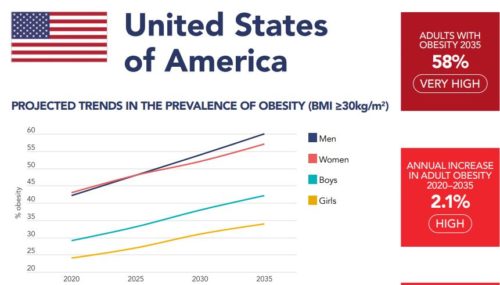
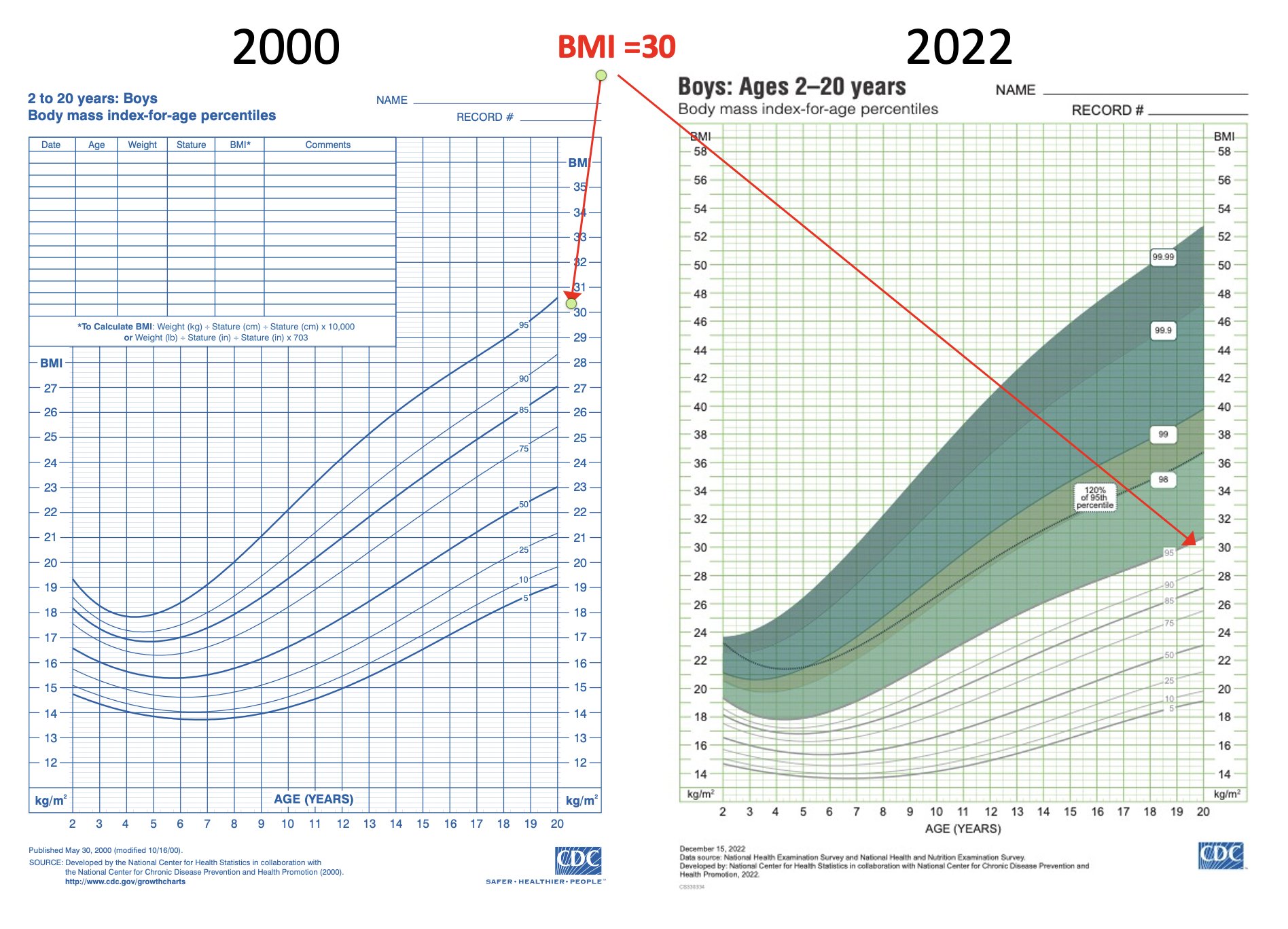
Three-quarters of American adults are overweight or obese and at increased chronic disease risk, yet nobody is screaming much about it (except for the MAHA people).
As the Government Accountability Office put it in 2021, “federal strategy needed to coordinate diet-related efforts.”
Chronic health conditions (like heart disease, diabetes, cancer, and obesity) are costly and deadly—causing over half of U.S. deaths in 2018. They also exacerbated the pandemic: Americans with such conditions were 12 times more likely to die after contracting COVID, according to the CDC.
Yet chronic conditions are largely preventable with a healthy diet and other behaviors like exercise. The federal government leads 200 different efforts, spread across 21 agencies, to improve Americans’ diets. But agency efforts are fragmented and there are gaps in key scientific research, including for children. A strategy for working together could help.
In its recommendations, the GAO says:
Congress should consider identifying and directing a federal entity to lead development and implementation of a federal strategy for diet-related efforts aimed at reducing Americans’ risk of chronic health conditions.
The GAO comments:
The White House sponsored a conference on Hunger, Nutrition, and Health on September 28, 2022. In advance of that event, the White House released a national strategy aimed at ending hunger in America and increasing healthy eating and physical activity by 2030. [Note: I wrote about these events extensively. For example, here]
However, we do not believe the White House strategy satisfies our matter because it does not contain the necessary information about outcomes and accountability, resources, and leadership. In particular, without designated leadership, it may be difficult to sustain the strategy over time. Therefore, as of March 2024, the matter remains open.
In October 2024, it still remains open. I see this as an urgent priority.
Tomorrow: Personalized nutrition