What do we need to know about bird flu?
[Oops. This one did not get sent out, apparently. Hope it works this time].
*****
The current bird flu pandemic is a huge worry, because the current strain, H5N1, is highly pathogenic .
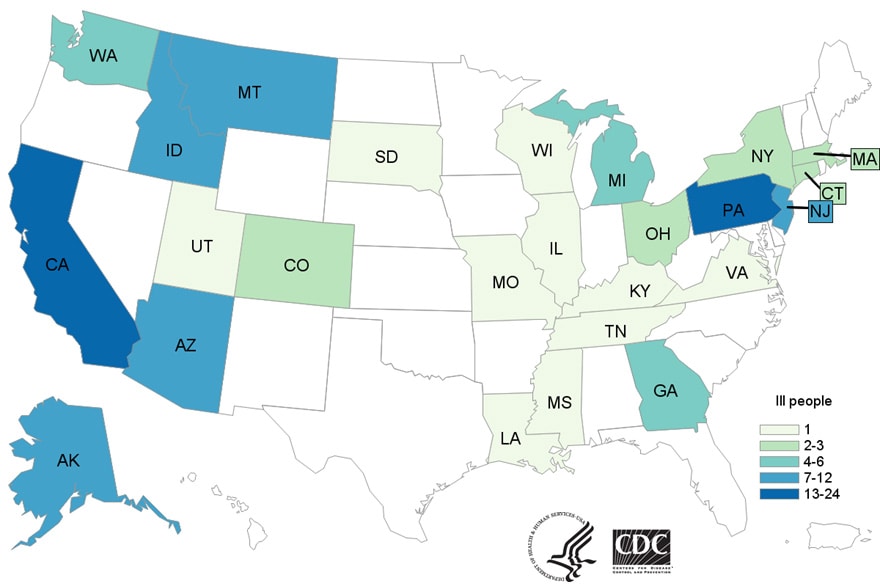
Although there have only been 4 reported cases in humans since 2022, the strain has infected:
- Nearly 100 million chickens .
- 101 herds of dairy cattle.
- Some number of cats
The CDC says: “Mammals can be infected with H5N1 bird flu viruses when they eat infected birds, poultry, or other animals and/or if they are exposed to environments contaminated with virus. Spread of H5N1 bird flu viruses from mammal to mammal is thought to be rare, but possible.”
Oh great.
The epidemiological fear, of course, is the more cattle affected, the more the virus can mutate (sound familiar?).
the personal fear is that the milk supply might contain active viruses. Untreated milk does, and lots.
But the NIH says tests show that the virus is destroyed by standard Pasteurization methods.
The FDA says (as it always has): do not drink raw milk.
This seems like especially good advice at the moment.
I’m going to be tracking this closely. Stay tuned.
Resources
- USDA’s home page for bird flu in livestock.
- USDA’s home page for detections of bird flu.
- CDC’s bird flu current situation page.
- CDC’s dairy herd situation page.
Also
The industry-fun Council for Agricultural Science and Technology (CAST) is doing a webinar , Highly Pathogenic Avian Influenza (HPAI) and Its Impact on Food Production Industries.” June 24 at 1 PM CST. Register for it here.