FDA’s food label proposals: comments on Vitamin D
The FDA is taking comments on label proposals until August 1 (see info at end of post). Here’s mine on voluntary vitamin D labeling.
July 17, 2014
TO: FDA
FROM: Marion Nestle, Professor, New York University
RE: Proposed revision to Nutrition Facts Panel: VITAMIN D
This is to argue against permitting food companies to voluntarily label added “Vitamin” D on the Nutrition Facts panel. Doing so will not promote—and may possibly harm–public health.
Rationale
- “Vitamin” D is not a vitamin; it is a hormone synthesized by the action of sunlight on skin. For this reason alone, it does not belong on the food label.
- Vitamin D fortification must be understood as a form of hormone replacement therapy. As such, it raises questions about efficacy, dose, and side effects that should be asked about all such therapies.
- Fortification and supplementation provide hormone Vitamin D by the oral route. This is not physiological. Active vitamin D is synthesized in the body through a series of reactions that begin with the action of sunlight on skin. Sunlight on skin produces ample Vitamin D, is regulated to promote synthesis as needed and avoid toxicity, and may lead to synthesis of other useful biological components; the unphysiologic oral route does not produce the same benefits.[i]
- As a hormone, Vitamin D is found naturally in very few foods (e.g., fish); in them, it is present in small amounts. It is present in most foods as a result of fortification.
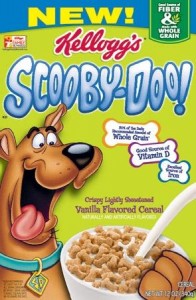
- Permitting Vitamin D to be listed on food labels will encourage fortification, undoubtedly of foods that would not otherwise necessarily be recommended. To cite just one example: Yum Bunny Caramel Milk Spread fortified with vitamin D at 10% of the DV. This product is half sugars by weight, marketed as “a good source of calcium and vitamin D,” and clearly aimed at children. See: http://www.yumbunny.com/about-us. Whether such products should be considered “good sources” also deserves scrutiny.
- The U.S. Preventive Services Task Force concludes that evidence is insufficient to determine how Vitamin D supplementation (and, therefore, fortification) affects fracture incidence.[ii],[iii],[iv]
- Data from the Women’s Health Initiative also are consistent with largely inconclusive findings about hormone Vitamin D supplements and bone health.[v]
- The Institute of Medicine (IOM) does not consider deficiency of Vitamin D to be a serious problem in the United States, except among certain population groups. Instead, because of widespread fortification and supplementation, it is concerned about the possibility of adverse consequences from overconsumption through supplementation or fortification.[vi]
- Many scientific debates about hormone Vitamin D are as yet unresolved.[vii],[viii]
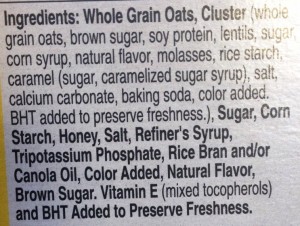
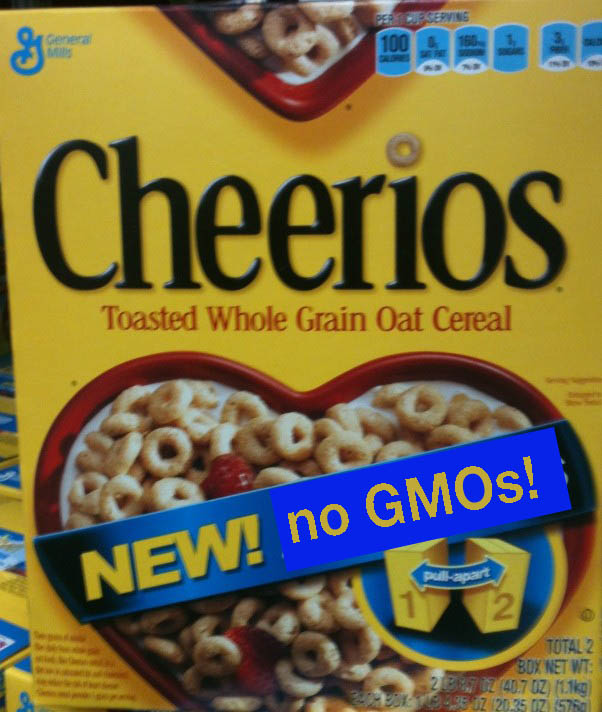
- The lack of compelling research has permitted Vitamin D to become “trendy.” It is advertised on boxes of fortified cereals, has its own pro-supplement advocacy group, and generates millions in annual supplement sales.[ix]
In the absence of stronger evidence for benefit from fortification, and some evidence for possible adverse consequences, the FDA should not contribute to further commercialization of this misnamed hormone by permitting it to be listed on food labels.
References
[i] Wacker M, Holick MF. Sunlight and Vitamin D: A global perspective for health. Dermato-Endocrinology 2013;5(1):51–108.
[ii] Cranney A, Horsley T, O’Donnell S, Weiler H, Puil L, Ooi D, et al. Effectiveness and safety of vitamin D in relation to bone health. Evidence Report/Technology Assessment No. 158. Rockville, MD: Agency for Healthcare Research and Quality. 2007. http://www.ncbi.nlm.nih.gov/books/NBK38410. Accessed February 5, 2013.
[iii] Chung M, Balk EM, Brendel M, Ip S, Lau J, Lee J, et al Vitamin D and calcium: a systematic review of health outcomes. Evidence Report/Technology Assessment No. 183. Rockville, MD: Agency for Healthcare Research and Quality. 2009. http://www.ncbi.nlm.nih.gov/books/NBK32603/. Accessed February 5, 2013.
[iv] Chung M, Lee J, Terasawa T, Lau J, Trikalinos T. Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155(12):827-38.
[v] Prentice RL, Pettinger MB, Jackson RD, Wactawski-Wende J, LaCroix AZ, Anderson GL, et al. Health risks and benefits from calcium and vitamin D supplementation: Women’s Health Initiative clinical trial and cohort study. Osteoporosis Int. 2013;24(2):567-580.
[vi] Institute of Medicine. Dietary Reference Intakes: Calcium, Vitamin D. Washington, DC: National Academies Press, 2011.
[vii] Rosen, Clifford J, Abrams, Steven A, Aloia John F. et al. IOM Committee members respond to endocrine society vitamin D guideline. J Clin Endocrinol Metab. 2012;97:1146-1152.
[viii] Holick, Michael F, Brinkley Neil C, Heike, A et al Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab. 2012;97:1153-1158.
[ix] Much growth in vitamin sales driven by vitamin D. Nutr Business J. 2009;14(6/7):5.
Here’s how to file comments:
The proposed revisions are to:
The FDA makes it very easy to file comments. It provides:
File comments here