The Physicans Committee for Responsible Medicine (PCRM), a group advocating against use of animals in research but for vegetarian and vegan diets, has started a campaign to restore egg-and-cholesterol recommendations to the Dietary Guidelines for Americans.
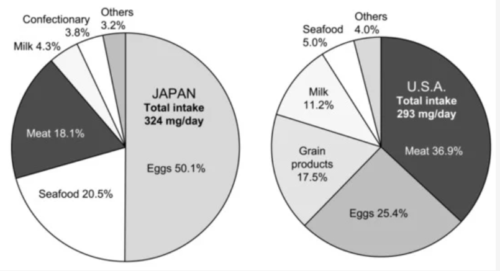
Eggs are the largest source of cholesterol in American diets.
The campaign involves billboards like this one, in six locations in Texas:

It also involves a new organization (truthaboutegg.org) with an interactive website on a dozen issues related to egg production and consumption.
The one that particularly caught my eye was #5.
A 2013 review suggested that high-cholesterol foods have only a modest effect on blood cholesterol. Of the 12 studies it relied on, 11 were industry-funded.
In a letter to Congressman K. Michael Conaway (Rep-TX), Dr. Neal Barnard, PCRM’s president, wrote:
This week, billboards near your Texas offices will alert you to the dangers Americans face if cholesterol warnings are removed…Eggs are the leading source of cholesterol in the American diet. A report (which I’ve included for your review) in the autumn 2015 Good Medicine magazine finds that this recommendation may have been influenced by egg-industry-funded cholesterol research. America’s heart disease and diabetes epidemics will continue unabated if the egg industry succeeds in its efforts to get cholesterol warnings out of the guidelines.
The 2015 Dietary Guidelines Advisory Committee (DGAC) said this about dietary cholesterol.
Cholesterol. Previously, the Dietary Guidelines for Americans recommended that cholesterol intake be limited to no more than 300 mg/day. The 2015 DGAC will not bring forward this recommendation because available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol, consistent with the conclusions of the AHA/ACC report.2,35. Cholesterol is not a nutrient of concern for overconsumption.
The DGAC based its unconcern about dietary cholesterol on two references:
2. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76-99. PMID: 24222015. Its conclusion:
There is insufficient evidence to determine whether lowering dietary cholesterol reduces LDL–C.
35. Shin JY, Xun P, Nakamura Y, He K. Egg consumption in relation to risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(1):146-59. PMID: 23676423. This study, which was also independently funded, concluded:
compared with those who never consume eggs, those who eat 1 egg per day or more are 42% more likely to develop type 2 diabetes. Among diabetic patients, frequent egg consumers (ie, > 1 egg/d) are 69% more likely to have CVD comorbidity…This meta-analysis suggests that egg consumption is not associated with the risk of CVD and cardiac mortality in the general population. However, egg consumption may be associated with an increased incidence of type 2 diabetes among the general population and CVD comorbidity among diabetic patients.
Were these references based largely on studies funded by the egg industry? If so, PCRM is correct in arguing that the question of egg consumption and blood cholesterol levels merits much closer scrutiny and analysis than it is currently receiving.
What does a study funded by the egg industry look like? Here are two one from my recent collection:
The effect of a high-egg diet on cardiovascular risk factors in people with type 2 diabetes: the Diabetes and Egg (DIABEGG) study—a 3-mo randomized controlled trial, by Nicholas R Fuller, Ian D Caterson, Amanda Sainsbury, Gareth Denyer, Mackenzie Fong, James Gerofi, Katherine Baqleh, Kathryn H Williams, Namson S Lau, and Tania P Markovic. Am J Clin Nutr 2015; 101:705-713.
- Conclusion: High egg consumption did not have an adverse effect on the lipid profile of people with T2D [type 2 diabetes] in the context of increased MUFA [monounsaturated fatty acid] and PUFA [polyunsaturated fatty acid] consumption. This study suggests that a high-egg diet can be included safely as part of the dietary management of T2D, and it may provide greater satiety.
- Sponsor: Australian Egg Corporation
Dietary cholesterol and cardiovascular disease: a systematic review and meta-analysis. Berger, S., Raman, G., Vishwanathan, R., Jacques, P.F., Johnson, E.J., 2015. Am J Clin Nutr ajcn100305. doi:10.3945/ajcn.114.100305. Am J Clin Nutr August 2015
vol. 102 no. 2 276-294
- Conclusion: Reviewed studies were heterogeneous and lacked the methodologic rigor to draw any conclusions regarding the effects of dietary cholesterol on CVD risk. [Implication: suggestions that eggs might raise cardiovascular risk are unwarranted]
- Sponsor: Supported by USDA agreement 1950-51000-073 and the American Egg Board, Egg Nutrition Center. The funders did not have a role in the study selection, quality assessment, data synthesis, or manuscript preparation.